
It is about Kenneth. He is known as Kenny, not Ken. He makes sure that everyone knows it especially fairly new nurses in the dialysis unit like me. Kenny was diagnosed with chronic kidney disease 20 years ago. That was when his wife was still alive. He tells me that they expected it because he had polycystic kidney disease. Due to advancement in care for early stages of kidney disease, Kenny did not start dialysis until 8 years ago. That was after his wife’s death from colon cancer. He tells me he stopped taking care of himself.
It had been ages since I last saw a patient using a femoral dialysis catheter. This one is inserted in the femoral vein which is accessed from your groin. I know it sounds painful but believe me the pain is the least of anyone’s concern. For a renal nurse, a femoral catheter poses the greatest risk for infections. As you can visualise, it is too near to the private parts where a good number of microorganisms live.
Femoral catheters are not meant to be used for long, but Kenny has used his for two years now. That was not the initial plan. His plan with the Vascular Access Nurse (VAN) team was to have him use a fistula from the start. They created a fistula which clotted and died off. They created another which did the same thing. It was a dialysis mystery.
Rarely do fistulae just clot without a reason given the high pressure with which blood flows through them. Kenny was special. As if that was not enough, catheters inserted through the internal jugular veins on either side of the next also failed. The vascular, haematology and renal teams went to work on overdrive. Surely there was a reason why Kenny’s blood was acting the way it was.
Before going for the femoral catheter, investigations were done which showed that Kenny’s blood has a natural tendency to clot. It did not matter which tactic was used; he would end up with very thick blood necessitating clotting. The doctors swung into action and prescribed a blood thinning medication called Warfarin. Kenny has been on Warfarin since then.
It has been a challenge trying to balance the ability of blood to stay thin enough to allow for dialysis to happen, and the risk of severe bleeding from minor injuries of daily living. Consensus was arrived at that due to the constant problems of achieving adequate dialysis even while he is on Warfarin, another method of blood access must be fashioned. The renal team settled for a graft.
What is A Graft?
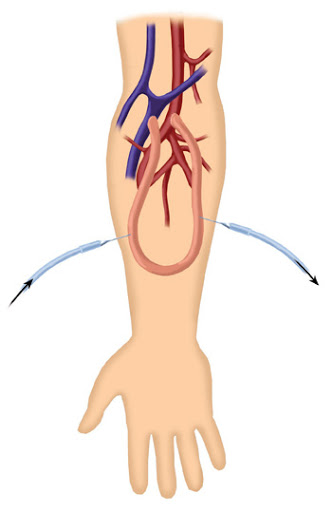
It is a small, hollow, synthetic tube that is placed in the arm to allow for blood access during dialysis. Grafts are made from different materials. The bottom line is that the material used is not harmful to the human body an cannot cause an allergic reaction.
How It works
Grafts are placed between an artery and a vein on the arm. They take time to get fully embedded in the skin. That gives room for nurses to start using them for dialysis. They are used like fistulae because they expand well enough to handle a high pump speed of the dialysis machine.
Either way, they are better than the femoral catheter that has been driving Kenny up the wall. He will have it fashioned next week after the procedure was cancelled many times due to the ongoing Covid-19 pandemic. I am excited for him and myself. For him because with a graft, he will get great dialysis treatment and for me because I will have yet another graft to practise my cannulation skills on. We learn every day, don’t we?
What Could Go wrong
Because grafts are synthetic juts like catheters, we have a risk of infection. This rarely happens with proper hand hygiene and regular monitoring. The graft can bleed or be injured if we do not have a skilled person putting in the needles. That is why nurses like me need continued practice on using grafts before we can be allowed to do it without supervision. It is all about what is best for Kenny.
Grafts can clot and believe me Kenny’s would easily clot if nothing had been done to address his usually highly viscous blood. Due to the joining of an artery and a vein using this graft, blood supply to the areas away from the graft could be cut off.
This is also the case with fistulae. The condition is called ‘Steal’syndrome. Perhaps because we have stolen blood from one artery, or a part of the artery and directed it to a vein. It comes as tingling sensation in the fingers, fingers feeling unnaturally cold or they may turn blue-ish or darker than usual. If this happens it is always important to let the nurse know. The renal nurses are your first contact on matters dialysis and kidney care. Renal nurses are a wealth of untold information on matters kidney health and ultimately, patient and family care while on dialysis.
SUMMARY
This blogpost has concluded the running series on blood access during dialysis. We agreed that the dialysis we are talking about is haemodialysis. The type where machines with pumps are used. It is also the most common type of dialysis in Kenya.
We discussed the following and these are the takeaways.
- Dialysis catheters: They are mostly used in cases of emergency. They have a very high risk of infection and are restrictive to the patient.
- Dialysis Fistulae: This is always the first line of blood access for a patient on dialysis. We discussed various styles of putting in the dialysis needles.
- We agreed that fistulae can easily cause massive bleeding after dialysis and that to prevent this, we must use a proper style of needling.
- We had a consensus that dialysis patients must take charge of their own treatment. Empowered to partake of the decisions of care that are made. This is because dialysis is a life term treatment in end stage kidney disease unless you get a kidney transplant.
- Transplants are not easy to come by even in first world countries like the United Kingdom.
- Grafts: They are not better than fistulae, but they are better than catheters. They also require skilled nurses to put the needles in so that they do not get damaged.
- Grafts can get various complications too and it is the role of the patient or the people taking care of them at home to bring any concern to the attention of the kidney nurse.
This has been a pleasure, thank you for following the series.
thank you for this,honestly I always look forward to your blogs.
You are welcome and thank you too.